A new study led by the University of Westminster has used predictive AI modelling techniques to anticipate whether cancer patients are likely to develop severe side effects if treated with radiotherapy to help potentially avoid treatment interruption and cancer recurrence.
The new collaborative research shows that through the use of predictive modelling and machine learning techniques, it is possible to understand whether a patient is likely to experience severe side-effects if treated with radiotherapy before initiating treatment. The research was a collaboration between the University of Westminster, University of Manchester and medical physicists, oncologists and surgeons from the UK Radiotherapy Machine Learning Network.
The study, which was recently published in Computers in Biology and Medicine, used AI machine learning techniques to investigate the health records of approximately 2000 cancer patients from 26 hospitals in the US and Europe, and these were split into two groups of radiotherapy side-effects incidence based on clinical observations from the REQUITE study. The researchers created and evaluated 80 machine learning models to assess these health observations and successfully built a predictive model to understand whether a cancer patient is likely to develop severe skin toxicity if treated with radiotherapy before initiating treatment.
Currently, radiotherapy physicists plan the treatment in protocols that include positioning, imaging, radiation doses and fractions so that it is effective and safe, and the tools they have do not account for the specific acute side effects happening to patients. However, this new Westminster-led research potentially promises medics a new tool in the future to fine-tune patient treatment plans even further and account for skin toxicity occurrence, so they may consider planning the treatment differently.
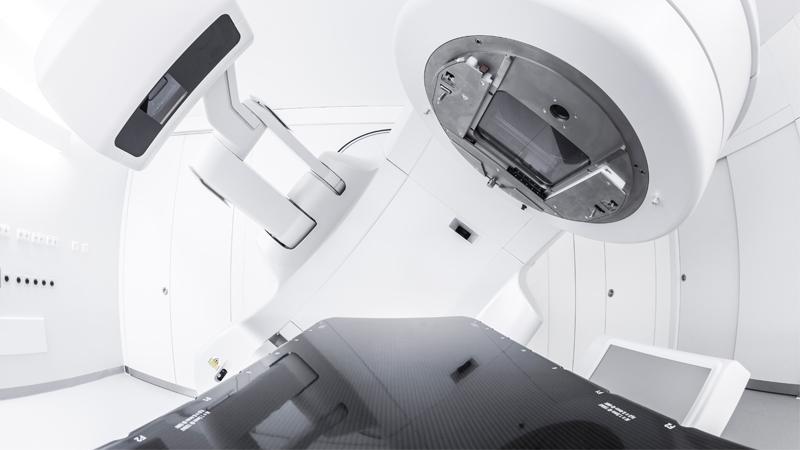
Cancer radiotherapy exposes malignant cancer cells to ionising radiation in doses, where radiation penetrates the body’s skin or organs to reach the target cancerous tumour and involved lymph nodes. While the treatment effectively damages the DNA of cancerous tissue leading to cellular death, it may severely impact the surrounding healthy skin tissue in some patients and causes them severe pain, ulcers, scars, liquid build-up under the skin, or other potentially life-threatening conditions. At present, there is no way to know who will get such side effects and who won’t.
As a result, in some cases, radiotherapy physicists are left considering two options of continuing the treatment while their patient endures such acute side effects or interrupting or discontinuing the treatment. However, if interrupted, the remaining cancer cells, after a halt, may become agitated, increasing the risk of cancer recurrence or even with a faster spread, reducing survival rates.
Talking about the research, Mahmoud Aldraimli, Lead Researcher and Health Data Science Research Fellow at the Health Innovation Ecosystem (HIE) at Westminster, said: “Collaborating with radiotherapy experts from the NHS is unquestionably an imperative bridge between the data science and radiotherapy communities. Additionally, conceiving findings which were covered by Action Radiotherapy, the UK’s only leading charity dedicated to improving radiotherapy treatment, confirms the potential robust connection that such a bridge can lead to in personalising patients’ treatments.”
Professor Thierry Chaussalet, Lead of the HIE and the Health and Social Care Modelling Group at Westminster, added: “It is fantastic to see our work being picked up so quickly by the leading charity dedicated to improving cancer treatment via radiotherapy, therefore having already an impact beyond academia towards clinical practice.”
Patients data was provided by the international study of RT related toxicity ‘REQUITE’, and the Radiotherapy Machine Learning Network was funded through the Advanced Radiotherapy Challenge and the Science and Technology Facilities Council (STFC). The work was also supported by the Health Innovation Ecosystem at Westminster and Quintin Hogg Trust, Cancer Research UK, the National Institute of Health Research (NIHR), Chief Scientist Office (CSO) and multiple other international funding bodies.
Read the full study in the Computers in Biology and Medicine journal.


