Dr Sigrun Lange, Senior Lecturer in Molecular Pathology, has led a new study identifying a novel pathway of regulating extracellular vesicles in glioblastoma brain cancer cells which can lead to improved treatment outcomes.
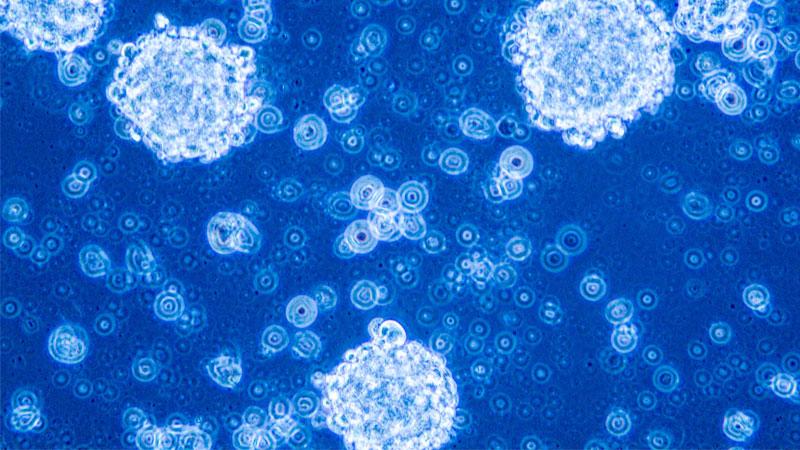
Identifying new pathways which can be targeted to make glioblastoma tumours less aggressive is imperative for improved treatment outcomes. One of the important factors contributing to glioblastoma spread and aggressiveness are extracellular vesicles, which are membrane vesicles released from cells.
These vesicles carry a lot of genetic and protein information from the cells they derive from and can therefore contribute to the progression and spread of cancers. Therefore, strategies to regulate these vesicles are a recent focus in cancer research, especially as standard treatments can sometimes induce the release of pro-cancerous vesicles, leading to less effectivity.
This study has identified a new way of regulating extracellular vesicles and modifying their cancer-inducing contents, making glioblastoma cells less aggressive.
Dr Lange and Dr Pinar Uysal Onganer worked on a group of enzymes called peptidylarginine deiminases (PADs), which cause specific protein modifications and control vesicle release in a range of cancers including glioblastoma multiforme (GBM), which is the most aggressive form of brain cancer.
This is the first study to assess specific effects of the different PAD enzyme forms in extracellular vesicle communication in glioblastomas.
The study shows significant effects of selective pharmacological inhibitors of the different PAD forms on the release and carcinogenic content of extracellular vesicles and on changes in the aggressiveness of different types of glioblastoma cells.
Glioblastoma multiforme (GBM) is an aggressive adult brain tumour with poor prognosis. One of the challenges in glioblastoma treatment is how diverse the tumours are. This makes them extremely difficult to treat and standard treatment with surgery, chemotherapy and radiotherapy have so far not led to satisfactory treatment outcomes.
Talking about the study, lead researcher Dr Sigrun Lange said: “We were quite surprised to find the strong selectivity that glioblastoma cells, which were derived from different patients, showed in the expression of specific PAD forms. This related directly to a significantly selective effect for the pharmacological PAD inhibitors targeting the corresponding PAD forms. Our findings highlight that we have identified selective PADs as important contributors to the notorious heterogeneity of glioblastomas.”
“It was quite striking how effectively PAD-inhibitors, aimed at the different PAD forms, could selectively change extracellular vesicle signatures in these glioblastoma cells to more anti-cancerous signatures and also make them less aggressive. The application of such tailored PAD-selective inhibition could therefore be a new strategy to target glioblastoma sub-types and for personalised approaches in glioblastoma treatment.”


